Connect With Us

Heel Spur Information

A heel spur is a bony growth that forms on the underside of the heel bone, often causing significant discomfort. This condition typically arises from repetitive stress or strain on the foot, which can lead to inflammation of the plantar fascia, the ligament that supports the arch. Risk factors can include obesity, prolonged standing, improper footwear, and activities that put excessive pressure on the feet. The main symptom is sharp, stabbing pain in the heel, particularly during the first steps in the morning or after periods of rest. To prevent heel spurs, it is essential to wear supportive shoes, maintain a healthy weight, and avoid excessive strain on the feet. Stretching exercises for the Achilles tendon and the plantar fascia can also help reduce the risk of developing this condition. If you have heel pain, it is suggested that you promptly schedule an appointment with a podiatrist who can accurately diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Michael Tomey, DPM from Cary Foot & Ankle Specialists. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Cary, NC . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Negatives of Wearing Flip Flops

Flip-flops, while convenient and casual, are not ideal for foot health. Their lack of arch support and cushioning can lead to issues like foot pain, poor posture, and increased risk of injury. The minimal support may worsen conditions like plantar fasciitis and contribute to misalignment of the feet. Flip-flops also offer little protection from sharp objects or uneven surfaces, making them unsuitable for extended walking or physical activities. They are best worn for brief periods in low-risk environments, such as the poolside or beach, where minimal foot protection is needed. For daily wear or activities that involve prolonged standing or walking, opt for footwear that provides proper arch support and cushioning to promote overall foot health and comfort. Foot conditions may develop when flip flops are frequently worn. If this applies to you, it is suggested that you consult a podiatrist for treatment and who can guide you toward more appropriate shoe choices.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact Michael Tomey, DPM from Cary Foot & Ankle Specialists. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our office located in Cary, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flip Flops and Feet
Flip flops are often a popular choice of footwear for many people. Flip flops allow your feet to breathe and give your toes the freedom of movement. They are easy to slip on and can be worn with virtually any style of clothing. Flip flops, however, despite their many benefits, can be detrimental for your foot health.
Despite their comfortableness, frequently wearing flip flops can create problems in the lower body over time. Issues mainly stem from the fact that people walk differently in flip flops compared to other footwear, such as sneakers. This is due to a change in one’s natural gait, which therefore creates stress in different parts of the body while hindering the body’s natural posture. Problems can also arise in the arches and balls of the feet. Flip flops provide little to no support to these areas.
Aside from long-term problems, flip-fops can also create short-term issues as well, such as ankle sprains and blisters. Weak materials that are flexible and bendable are generally used to manufacture flip flops. These materials make its wearers prone to both tripping and injuring their ankles. Flip flops can create blisters as the material rubs against the foot. People are much more at risk for infection while wearing flip flops due to their openness. This also makes it easier to scrape and cut the foot since there is a lack of protection. If these cuts are left untreated and uncovered, the risk then becomes greater.
To prevent the aforementioned occurrences, purchase a pair of flip flops that offer significant protection. The soles of the flip flops should not be floppy, but sturdy and firm, and should not significantly bend or wiggle when lifted from the floor. Flip flops made of high-quality materials will not be affected by this problem. While higher quality flip flops may be more expensive, they will last longer and provide better protection compared to a cheaper pair. Brand name flip flops sold from a quality manufacturer are a dependable option.
There is no problem in wearing your favorite pair of flip flops so as long as you do not wear them daily or for extended periods of time. Flip flops should be replaced every 3-4 months to ensure that they provide your feet with the best protection.
Minimally Invasive Achilles Tendon Surgery
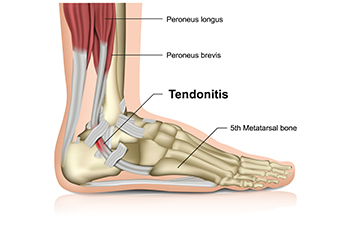 The Achilles tendon, the strongest tendon in the body, connects the calf muscles to the heel bone and is important for walking, running, and jumping. Achilles tendon injuries, such as ruptures, often result from sudden increases in activity or trauma. Conservative treatment for Achilles tendon injuries includes rest, compression, and elevation, in addition to immobilization with a cast or brace to allow natural healing. This approach is typically recommended for less severe injuries or for patients who may not be suitable candidates for surgery. Minimally invasive Achilles tendon repair surgery involves making small incisions to stitch the torn ends of the tendon together. This method reduces the risk of infection, minimizes scarring, and often leads to faster recovery times compared to traditional open surgery. Choosing between conservative treatment and surgery depends on the injury's severity, the patient’s activity level, and overall health. If you have injured your Achilles tendon, it is strongly suggested that you schedule an appointment with a podiatrist to help you determine the best course of treatment.
The Achilles tendon, the strongest tendon in the body, connects the calf muscles to the heel bone and is important for walking, running, and jumping. Achilles tendon injuries, such as ruptures, often result from sudden increases in activity or trauma. Conservative treatment for Achilles tendon injuries includes rest, compression, and elevation, in addition to immobilization with a cast or brace to allow natural healing. This approach is typically recommended for less severe injuries or for patients who may not be suitable candidates for surgery. Minimally invasive Achilles tendon repair surgery involves making small incisions to stitch the torn ends of the tendon together. This method reduces the risk of infection, minimizes scarring, and often leads to faster recovery times compared to traditional open surgery. Choosing between conservative treatment and surgery depends on the injury's severity, the patient’s activity level, and overall health. If you have injured your Achilles tendon, it is strongly suggested that you schedule an appointment with a podiatrist to help you determine the best course of treatment.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Michael Tomey, DPM of Cary Foot & Ankle Specialists. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Cary, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
Treat Your Feet to Diabetic Shoes
Treat Your Feet to Diabetic Shoes
Treat Your Feet to Diabetic Shoes
What Is Peripheral Neuropathy?

Peripheral neuropathy is damage to the nerves that are located outside of the brain and spinal cord, preventing communication with the extremities. Diabetes often causes peripheral neuropathy. However, it can also occur due to genetics, infections, injuries, hormonal imbalances, or other medical conditions. Peripheral neuropathy may cause numbness, weakness, muscle twitching, or cramps in the feet. It may also cause changes in nails, skin, and hair, and often results in a pins-and-needles sensation in the legs and feet. Peripheral neuropathy may affect the balance and prevent your ability to recognize temperature changes or pain. You may also experience disturbances in your emotions and sleep patterns. If you have any of these symptoms, it is suggested you contact a podiatrist. They can help diagnose peripheral neuropathy and manage its symptoms with oral medications, orthotic devices, regular checkups, and advice on proper foot care.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Michael Tomey, DPM from Cary Foot & Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Cary, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.